Update: IAPCON 2022, Jaipur – Day 2
The Quest for Knowledge continued on Day 2 of IAPCON 2022
The palliative care community continued to quench their thirst for knowledge as IAPCON 2022 progressed to Day 2 of the three day academic fiesta.
A total of 10 sessions were delivered virtually from both of the conference halls.
The IAPC’s Annual General Body Meeting was also held virtually between 11:30 a.m. and 1 p.m. on the same day.
Please find below a summary from the sessions from IAPCON 2022 delivered on 12th February, 2022.
We thank all our dear contributors (Dr Babita Varkey, Dr. Dipankar Dakua , Dr Jyothsna Kuriakose, Dr Krithika Rao, Dr Nimisha Verma, Dr Praneeth Suvari, Dr Pooja Mongia, Dr Priyadarshini Kulkarni, Ms. Sangeetha N, Dr Seema Partani and Dr Shrikant Atreya) for their support in sharing content towards this report!
1. Session name: Orphan Symptoms
Chairpersons:
Dr T Mohanasundaram (Palliative Care Consultant and President of Tamil Nadu Palliative Care Society)
Dr Tony Vikas Bishwas (Palliative Care Consultant, Christian Institute of Health Sciences and Research, Dimapur, Nagaland)
Moderator:
Dr Dipankar Dakua (Palliative Care Consultant, Department of Pain & Palliative Care, Assam Cancer Care Foundation, State Cancer Institute, Guwahati, Assam)
The session on Orphan Symptoms began with Dr Yoshiyuki Kizawa’s (Designated Professor and Chair, Department of Palliative Medicine, Kobe University School of Medicine) session on ‘Tenesmus’. This was followed by Dr Ghauri Agarwal’s (Associate Professor and Head, Concord Centre for Palliative Care) presentation on ‘Xerestomia’. Dr Mahesh Menon’s (Consultant, Bahrain Oncology Centre) lecture on ‘Hiccups’ concluded the session.
The speakers shared that Orphan Symptoms were those symptoms which are not regularly assessed in clinical practice and are consequently studied less and not treated properly. They went on to add that symptoms such as Tenesmus, Xerostomia, Hiccups, etc. remain unaddressed in clinical practice if they are not highlighted by the patient or not specifically sought by the healthcare professional themself. They concluded by saying that these symptoms would probably significantly impact the quality of life of patients’ if not treated with outmost importance.
2. Session name: Palliative Care in Covid
Session Lead: Dr Seema Rao (Associate Director, Education & Research, Karunashraya, Bengaluru)
Chair persons:
Dr Sudhir Bhandari (Principal and Controller, SMS Medical College, Jaipur)
Dr Ankit Bansal (Senior Pulmonologist and Intensivist, Fortis Escorts Hospital, Jaipur)
Moderator:
Dr Krithika Rao (Assistant Professor, Department of Palliative Medicine & Supportive care, Kasturba Medical College (KMC), Manipal)
The session commenced with Dr Seema Rao presenting a brief introduction about the COVID-19 pandemic and the experiences gained from Udupi, a small town in Karnataka. She shared that the challenging situation forced clinicians and hospital administrators (from KMC, Manipal) to develop a rapid response to tackle the unfurling crisis and to ensure that patient’s received appropriate management while the team judiciously utilized the available resources.
The COPE-CP pathway was therefore developed to provide Palliative Care & End-of-Life care in patients with serious COVID-19 illness. A rapid review of the outcomes of implementing the COPE-CP pathway was published in the Indian Journal of Palliative care.
A panel represented by Dr Shwethapriya R (Professor, Department of Critical Care Medicine, KMC, Manipal), Dr Vishal Shanbhag (Assistant Professor, Department of Critical Care Medicine, KMC, Manipal) and Drs Pankaj Singhai and Krithika Rao (Both AssistantProfessors’, Department of Palliative Medicine & Supportive Care, KMC, Manipal) discussed cases seen in the hospital during the pandemic and shared the challenges faced and the responses to those issues. They also touched upon the decision-making process, the referral to in-hospital palliative medicine team, communication challenges with familes and the need of the hour adaptations.
The take home points from the session as below:
- Palliative Medicine was recognized as an essential aspect of care in this humanitarian crisis with a shift in attitude and perceptions about palliative medicine amongst the Critical Care Providers and Physicians from other specialties
- Integration of critical care and palliative care (PC) during humanitarian crisis alleviated serious health-related suffering of patients and their families
- Honest and open communication across healthcare teams (via joint team meetings) and the patients’ family allowed for better decision making, both for the medical team and the family.
- The COPE-CP incorporated the core principles of team-based healthcare. It defined shared goals, provided clarity of roles, fostered mutual trust and established channels for effective communication between the members of interdisciplinary team.
- A patient’s palliative care needs were therefore identified timely and appropriate management was provided
- There was general acceptance about decision making on medical futility and discussions around Withholding or Withdrawal of Life sustaining treatment ensued
3. Session name: What’s in a Name? Should we change the name: Palliative Care?
The much awaited and hugely popular annual debate of IAPCON 2022 was a session that was not to be missed at IAPCON 2022.
Dr Shrikant Atreya (Senior Consultant, Department of Palliative Care and Psycho-oncology, Tata Medical Center, Kolkata) and Dr Jyothsna Kuriakose (Senior Resident, Department of Palliative Medicine, Tata Memorial HospitaI, Mumbai) moderated the mind boggling and scintillating session in which young palliative care physicians debated on the conundrum, ‘Should we change the name of our (Palliative Medicine) specialty.’
Dr. Prasun P, Dr. Raghav Gupta, Dr. Rutula Sonawane, Dr. Sarita Singh and Dr. Somnath Dey presented their arguments in favour of a name change, while, Dr. Jyotiprakash Samal, Dr. Krithika S Rao, Dr. Manasi Patil, and Dr. Vijayender Goud presented their arguments against changing the name of our specialty.
Each participant was allowed 5 minutes to rest their case and at the end of 50 minutes, conference delegates were asked to share their opinion and thoughts on the said subject. Interestingly, a revelation of mixed opinions emerged which revolved around the attitudinal shift and change of one’s perspectives.
All 9 participants presented the conference delegates with a riveting and thought provoking debate session.
Dr Krithika S Rao from Kasturba Medical College, Manipal was awarded the first place in the competition while Dr Raghav Gupta from AIIMS New Delhi, secured the second place in this interesting debate session.
4. Session name: Plenary 2
Chair persons:
Dr. Sukdev Nayak (Professor, Department of Anaesthesiology, AIIMS Bhubaneswar and Former President, IAPC)
Ms. Poonam Bagai (Founder Chairman, CanKids KidsCan, New Delhi)
Moderator:
Dr Priyadarshini Kulkarni (Palliative Care Consultant, Pune and Former Secretary, IAPC)
The Plenary provided delegates with a unique opportunity to listen to the very eminent and pioneer faculty of Palliative Care in India, Dr. Lucito deSouza (Founder and Managing Trustee, Shanti Avedna Sadan) and Dr M R Rajagopal (Founder and Chairman, Pallium India).
Dr deSouza in his enlightening speech on ‘My experience of palliative care in last 40 years’ reflected on his journey in Palliative Care. He shared the reasons for his motivation and how he decided to take the plunge and begun palliative care in India through Shanti Avedana to add life to the days of terminally ill patients. He cited several real-life examples, and shared a few real-life lessons that he learnt during his journey. One of the pearls of wisdom he shared with the delegates was, “Be gentle, listen to the patient, show empathy, and display competence with compassion; and don’t forget that the final goal is to bring peace”.
The delegates were in for further delight as Dr. M.R. Rajagopal delivered yet another brilliant talk on ‘If you can’t measure it, you can’t improve it. Indicators for access to palliative care’. While throwing light on the need to focus on quality, he also emphasized the importance of various process and output measurements. Dr Rajagopal went on to share a few key milestones which denoted the progress of palliative care in the country. The milestones included the launch of the National Program for Palliative Care (2012), the amendment to the Narcotic Drugs and Psychotropic Substances Act (2014), the inclusion of palliative care in the National Health Policy of 2017, the integration of palliative care into the MBBS curriculum (2019) and the integration of palliative care into the nursing curriculum (2021). Dr Rajagopal concluded by advocating for improved community engagement to foster awareness, increase participation and ultimately improve access to services.
5. Session name: Good Death
Moderator:
Dr Babita Varkey (Associate Medical Director, Karunashraya, Bengaluru)
Chairpersons:
Dr. Stanley Macaden (Honorary Palliative Consultant, Bangalore Baptist Hospital, Lead – Project India for International Collaborative for the best care of the Dying Person, University of Liverpool UK)
Dr. Dinesh Goswami (Founder, Secretary of Guwahati Pain and Palliative Care Society, and IAPC Faculty)
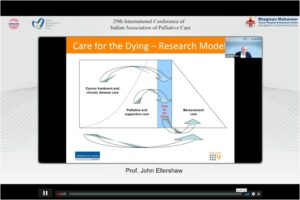
Prof. John Ellershaw’s (Head, Palliative Care Unit, Supratheme Lead for Core Skills, School of Medicine, University of Liverpool, Institute of Life Course and Medical Sciences) presentation on ‘Best care of the dying’ highlighted the current aspects of care provided for end of life patients and how International Collaborative was trying to bring about good End of Life Care practices. He also spoke about ‘Project India’.
Dr Chong Poh Heng’s session (Medical Director, HCA Hospice Care, Singapore), on ‘Dying in a Seriously ill Child’ presented about End of life care planning in Paediatric patients and highlighted the current practices in Pediatric Palliative Care.
The last presentation in this session was delivered by Dr Eric Finkelstein (Executive Director, Lien Centre for Palliative Care, and Professor in Health Services and Systems Research Program, Duke-NUS Medical School, Singapore). Dr Finkelstein presented on ‘Quality of Death and Dying Index 2021: A Preference-Based Approach’. He expressed that “the factors that patients, caregivers, and health professionals believe in are important at end of life. We used something called a discrete choice experiment (DCE) to measure the relative value of these factors” and that the study looked at indicators which are important at the end of life like managing pain, safe spaces, treated with kindness etc. along with the relative importance of each of these factors.
6. Session name: Effective Leadership in Palliative Care
Chairperson:
Dr Seema Mishra (Professor, Department of Onco anaesthesia and Palliative Medicine, AIIMS New Delhi)
Moderater:
Dr Seema Partani (Palliative Care Physician and Professor, Department of Anaesthesia, Geetanjali Medical College, Udaipur, Rajasthan)
This session highlighted the role of leadership in multi-professional PC team and its importance in effective coordination and motivation of team members to achieve sustainable and effective palliative care services.
Dr Fiona Rawlinson’s (Director, Cardiff’s Development and Alumni Relations Department, and Member, Executive Board, Cardiff University) session on ‘Need for Leadership in Palliative Care’ enlightened delegates with the theoritical aspects to explore strategies for enhancing leadership, the various communication styles and the Cardiff’s 6-point tool kit for reflective practical framework.
Dr Priyadarshini Kulkarni’s (Palliative Care Physician, Pune) presentation on ‘Team work and Leadership’ provided delegates with practical tips for leadership and highlighted that a team achieved more while working together. She went on to add that a good leader empowers people, inspires people to lead change with shared vision and decreases the work load by creating a leader in every team member for effective and sustainable goal directed palliative care services in a holistic approach.
The session was concluded by highlighting that Leadership in Palliative Care was rewarding, exciting, challenging and empowering to further develop palliative care.
7. Session name: From the journal to the bedside-Knowledge translation
Chairpersons:
Dr. Rajashree K.C (Assistant Professor, Amrita Institute of Medical Sciences, Kochi)
Dr. Farzaana Khan (CEO and President, Fasiuddin Khan Research Foundation Dhaka, Bangladesh)
Moderator:
Dr. Praneeth Suvvari (Consultant, onco-anaesthesia, Pain and Palliative Care, Basavatarakam Indo American Cancer Hospital and Research Institute, Hyderabad)
Dr Odette Sprujit’s (Founder, Australasian International Palliative Link, Associate Professor, University of Melbourne) session on ‘Relationship-Centered Care’ highlighted the importance of the Relationship dimension in Health Care to relieve suffering. Dr Sprujit shared that most of the available evidence in this area focused on geriatric population and that the United States of America contributed to 71% of global research. She also shared that the way in which clinicians and patients viewed each possibly influenced the direction of an interview and the data elicited and that sharing Predetermined designations of clinicians affected dimensions such as mood, thought process, content, insight and judgment.
Dr Naveen Salin’s (HoD, Department of Palliative Medicine and Supportive Care, Kasturba Medical College and Hospital, Manipal) session on ‘Using Theory of Change Framework to enhance ICU Palliative Care Engagement in India’ highlighted that Change was a response to external influence in which modifying day-to-day actions achieved desired results, whereas Transformation was about modifying care beliefs and long term behaviors to achieve the desired results. He also enlightened the delegates about the MRC (Medical Research Council) UK’s complex intervention research cycle.
Dr. Anil Paleri’s (Clinical Director, Palliative Care Services, Kozhikode, and Consultant, WHOCC for Community Participation in Palliative Care and Long Term Care, Institute of Palliative Medicine) session on ‘Evidence for use of Corticosteroids in Advance Cancer’ was the last presentation in this session. Dr Paleri reported the presence of strong evidence for use of steroids only in cases of raised ICP, whereas moderate evidence existed in the case of spinal cord compression, and tentative evidence in bowel obstruction, lymphangitis carcinomatosis, Superior Vena Cava obstruction and large airway obstruction. He added that we were not yet aware of the effectiveness of steroids in Liver metatstasis, obstructive lymphadenopathy and bronchorrhoea and that there was strong evidence about monitoring of blood sugars when a patient was started on steroids.
The key points from the session were therefore,
- Practicing Relationship centered care can establish practice settings that focus on patient/family in care planning
- Implementing the Theory of Change Framework enhances early palliative care conversation with patients and families and can thereby improve quality of death among patients.
- There is no available evidence that the use of Dexamethasone could disrupt Circadian Rhythm and sleeping patterns.
8. Session name: Nurses in Action – Best Practices in Empathy and Empowerment
Chairpersons:
Lt. Alice Stella Verginia (Retd. Army Nurse, National Faculty for palliative care, and a Faculty for the National Program in Palliative Care, Government of India)
Dr. A Latha (Tutor, College of Nursing, AIIMS Jodhpur)
Ms. Neelima Sharad Shingade (Senior Nursing Officer, AIIMS New Delhi)
Moderators:
Ms. Sangeetha N (Nursing Tutor, Karunashraya, Bengaluru)
Ms. Anu Thelly (Nurse Consultant, Department of Palliative Medicine, Mahathma Gandhi Medical College & Research Institute, Pondicherry)
Mr. Terrymize I (Palliative Care Coordinator / Staff Nurse, Christian Fellowship Hospital, Oddanchatram)
This session was organized exclusively for nurses to explore the challenges they face while performing difficult Nursing procedures in seriously ill patients. The practical session was delivered by seven eminent nursing faculties [Ms Ajisha Abhilash (Amrita Institute of Medical Sciences, Kochi), Ms Avanigadda Durgabhavani (Staff Nurse A, Homi Bhabha Cancer Hospital and Research Centre, Visakhapatnam), Ms Mamta Parihar (Lecturer, DR. S N Medical Government Nursing College, Jodhpur), Ms Meheli Chakraborty (CEO, Ruma Abedona Hospice), Ms. Shakila Murali (Charge Nurse, Christian Medical College, Vellore), Ms Shiny (Staff Nurse and Training Faculty, Institute of Palliative Medicine) and Ms Sumitra (Senior Staff Nurse, Ward in Charge, Bhagwan Mahaveer Cancer Hospital & Research Centre, Jaipur)] from across the country who demonstrated the various nursing procedures.
The Faculty shared practical tips and tricks gained over years of practice. Delegates pointed out that nurses from across the country benefitted immensely as they learnt about several nursing procedures in a structured and stepwise manner, which followed standard protocols and guidelines which would definitely help them to provide quality care to their patients.
The key takeaway points from the session included:
- Ways to perform nursing procedures in different palliative care settings like inpatient, home care, OPD etc.
- Importance of adopting evidence-based practices for better outcomes
9. Session name: Research in palliative care: Increasing the odds of publication
Chairpersons:
Dr. Ravi Prasad Varma (Additional Professor, Achutha Menon Centre for Health Science Studies, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum)
Dr. Santosh Chaturvedi (Consultant Psychiatrist, Leichester, UK)
Moderator:
Dr Pooja Mogia (Assistant Consultant, Bhagwan Mahaveer Cancer Hospital and Research Centre, Jaipur)
The session began with Dr Catherine Walshe’s (Professor, Palliative Care, International Observatory on End of Life Care, Lancaster University, UK) session on ‘Gaps in Palliative Care research: Asking the right question?’ which introduced delegates on how to define a research problem. She also recommended that a research problem be defined and derived from one’s own knowledge and from available literature.
Dr Raghavendra Ramanjalu (Lead Consultant, Head, Pain, Palliative, Rehabilitation Medicine, Aster Group of Hospitals, Bengaluru) in his session on ‘Appropriate design and methodology’ then went on to add that having well laid out and a detailed methodology will most certainly lead to efficient research.
The next speaker, Dr Rakesh Garg (Additional Professor, Department of Onco Anasthesia and Palliative Medicine, AIIMS New Delhi) the presented on ‘Basic Statistics and Analysis’ in which he urged delegates to not over emphasize the p-value and to make efforts to understand the statistics right from the project inception. Dr Garg suggested that it would be worthwhile to include a statistician on the team right from the beginning.
Dr Jennifer Jeba (Professor and Head, Palliative Care Unit, Christian Medical College and Hospital, Vellore) in her session on ‘Writing well – sharing the research story’ emphasized that researchers need to ensure that a manuscript must be presented like a story for maximum impact.
This session concluded with Dr Raghu Thota’s (Professor, Department of Palliative Medicine, Tata Memorial Cancer Hospital, Mumbai) session on ‘Editor’s Perspective’ in which he shared insights from the lens of an editor reviewing articles. Dr Thota shared that researchers needed to invest time to choose the right journal, avoid plagiarism and salami slicing and avoid repetition of ideas and concepts.
The take home points from the session was that Good researches are those which include a good review of literature, have a clear research problem and have a well defined and detailed methodology
10. Session name: Setting up a Palliative Care Program
Chairpersons:
Dr Maya Mascarenhas (Consultant, NHSRC)
Dr Suresh Kumar (Director, WHO Collaborating Centre for Community Participation in Palliative Care and Long term Care, Institute of Palliative Medicine)
Moderator:
Dr Nimisha Verma (Associate Professor Anesthesiology, Institute of Medical Sciences, Banaras Hindu University Varanasi)
This very interesting session was delivered by three wonderful speakers, Dr Savita Butola (Honorary Secretary, IAPC), Dr Mallika Tiruvadanan (Specialist, Palliative Medicine, and Founder of Lakshmi Pain & Palliative Care Trust, Chennai) and Dr Republica Sridhar (Founder and Managing Trustee, RMD Pain and Palliative Care Trust, Chennai).
The speakers vividly discussed and represented perspectives from different palliative care service delivery models viz government hospitals, charitable setups and corporate hospitals.
The Key points from the session as below:
- Focus must always be directed to the patient
- Creating public awareness is crucial
- Networking is vital
- Effective preliminary work is mandatory and needs to factor in local context
- Advocacy with key stakeholders is beneficial
- Never be ashamed to engage in fundraising and ask for money – it is for a cause
- Palliative care is all about employing low technology with a high touch component.
- Partnership is the way forward and not criticism or competition